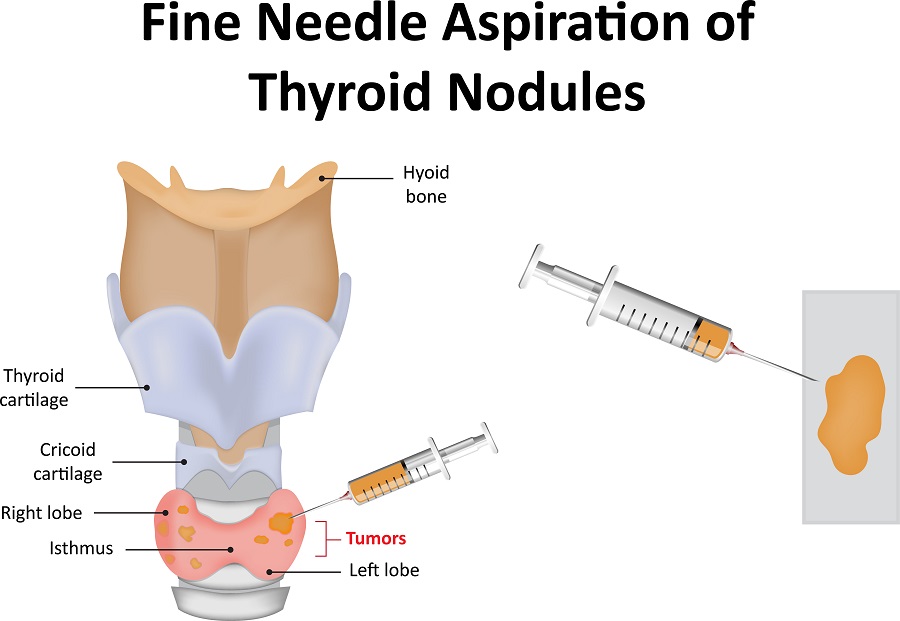
Thyroid nodules are fairly common in adults and etiology of nodules is widely variable. Population studies have shown the prevalence of palpable thyroid nodules in about 5% of women in iodine deficient regions and US finding of thyroid nodules has been reported in up to 60% of individuals with higher rate in women and elderly. Iodine deficiency, certain diets, medications, thyroiditis, familial syndromes, external beam radiation and neoplasms are potential etiologies of thyroid nodules. Evaluation should include physical examination including family history, blood work and diagnostic imaging when indicated. Ultrasound (US) of the thyroid and US guided fine needle aspiration biopsy (FNA) of the thyroid gland are the most important and widely used diagnostic tests used in evaluating thyroid nodules. Other diagnostic investigations such as CT scan, MRI, and nuclear imaging may be considered. On occasion thyroid nodules may be identified on positron emission tomography (PET-scan) and may convey an increased risk of thyroid cancer and require further evaluation.
US imaging of the thyroid nodules will determine the size, cystic vs. solid nature, characteristics (echogenicity, shape, presence of calcifications, vascularity, etc) and location of the nodules. It can also be helpful in evaluating the lymph nodes in the setting of thyroid cancer. The size and characteristic of the nodule determine if US guided FNA of the nodule is indicated. certain US characteristics such as solid composition, hypoechoic echogenisity, microcalcifications, irregular border, taller than wide nodules, extrathyroidal extension and suspicious nodes are associated with higher rates of malignancy. Generally, only nodules >1cm should be considered for biopsy. Only in rare situations, nodules less than 1cm need evaluation by biopsy.
FNA findings are reported based on the Bethesda system which has been shown to be helpful in estimating the risk of malignancy in the nodule:
| Diagnostic Category | Risk of malignancy (%) |
| Nondiagnostic or Unsatisfactory | 1-4 |
| Bening | 0-3 |
| Atypia of undetermined significance or follicular lesion of undetermined significance | 5-15 |
| Follicular Neoplasm or suspicious for follicular neoplasm | 15-30 |
| Syspicious for malignancy | 60-75 |
| Malignant | 97-99 |
The table is adopted from the report by Cibas ES, Ali SZ. The Bethesda system for reporting thyroid cytopathology. Am J Clin Pathol. 2009;132:658–65.
Treatment will depend on cytologic findings and diagnostic imaging and discussion with your physician. In the setting of AUS, FLUS, genomic testing in conjunction with cytologic evaluation may increase the predictive power with regards to cancer or benign diagnosis.