Lymphocintigraphy and Sentinel Lymph Node Biopsy
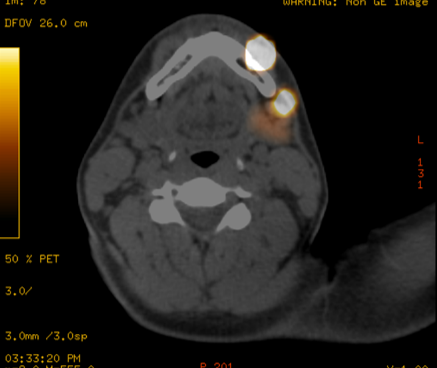
Each primary skin cancer site has a unique nodal drainage, and lymphocintigraphy can accurately predict the regional nodal basin and the unique initial draining lymph node (Sentinel lymph node). The concenpt of Sentinel Lymph Node Biopsy (SLNB) was first developed by Dr. Morton and Collegues ended the need for elelctive lymph node dissection and complexity of idetifying the draining lymph node basin. The status of the node is highly predictive of the entire nodal basin. However the hottest node (most radioacitive) is not always the positive sentinel node and for this reason it is recommended that all nodes with radioactive counts greater than 10% of the hottest node be resected for analysis. SLNB should be considered based on the depth of the primary melanoma and characteristics that were described above. Regional lymph nodes are the most common site of first recurrence.
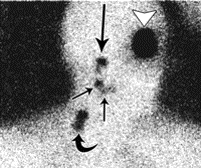
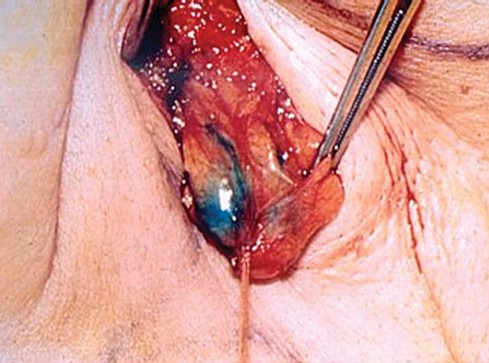
Lymphocintigraphy or lymph node mapping done the day beofre surgery or the day of surgery to locate the sentinel lymph nodes(s). Intradermal injections of 99mtechnetium-labeled (99mTc) sulfur colloid particle are made at the perimeter of the biopsy scar. All regional node bearing areas are scanned under the gamma camera. Sites of uptake are labled on the lymphocintigram. Intra operatively, blue dye may be injected intradermally at the biopsy marings to aid with the localization of the SLN. A hand held gamma probe is used during the surgery to aid with the localization and removal of the sentinel lymph node(s).
If the sentinel lymph node is positive for metastatic melanoma, completion compartment based lymph node dissection should be considered.